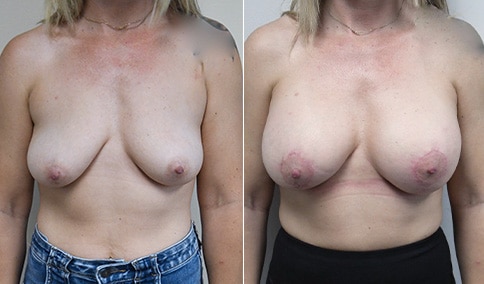
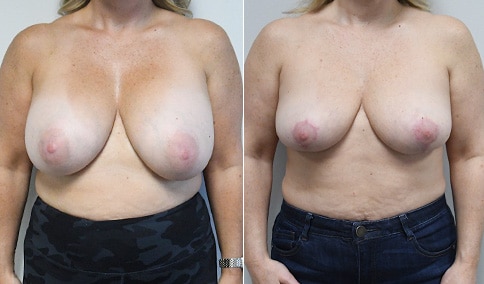
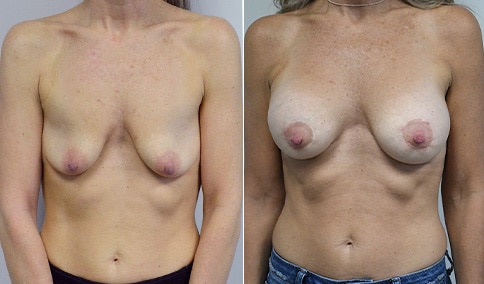
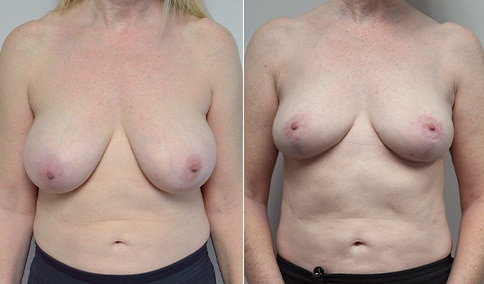
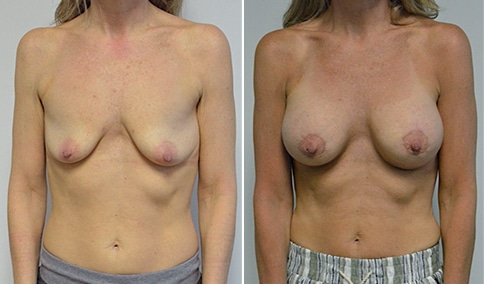
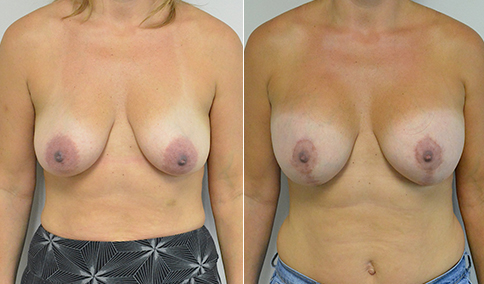
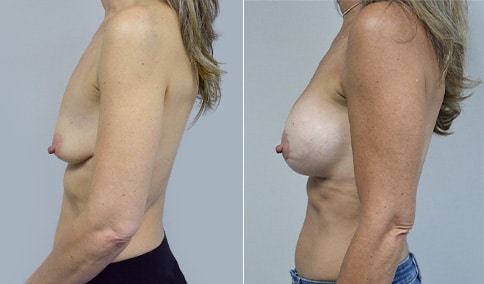
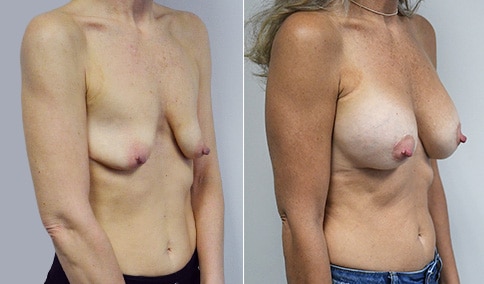
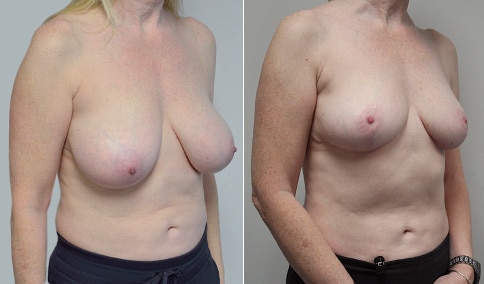
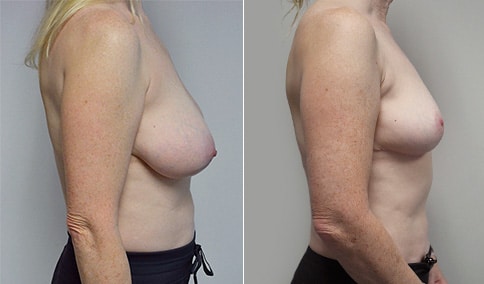
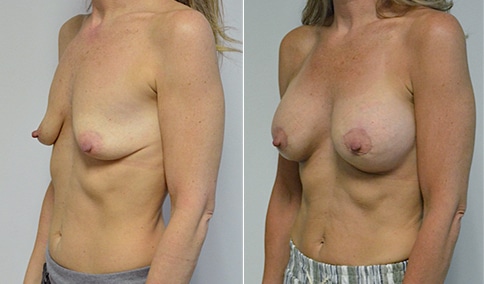
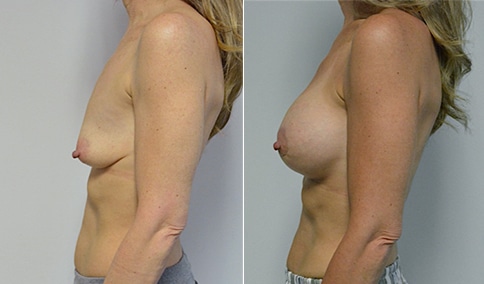
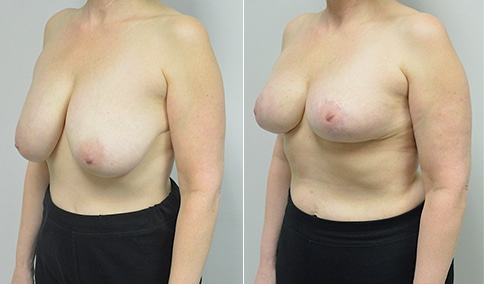
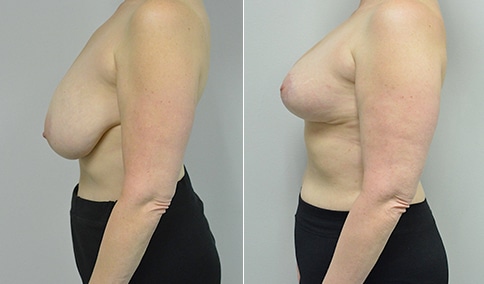
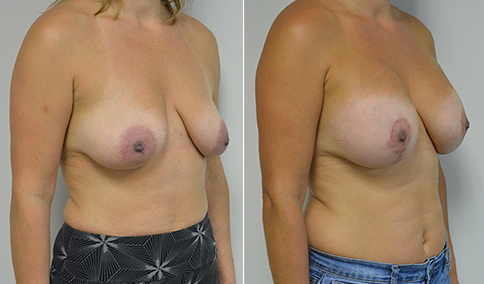
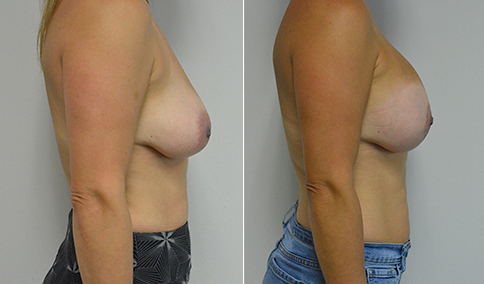
A mother of 3 in her mid 40’s who is bothered by the deflated look of her breasts after pregnancy and breast feeding. She would like to be fuller but still natural in appearance.
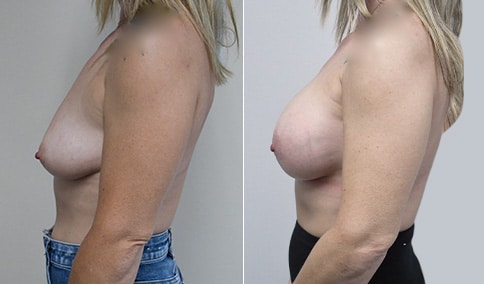
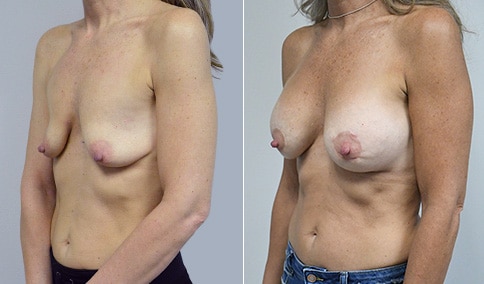
She is shown before and again, 6 weeks after augmentation/mastopexy. She is 5’3” and 111 lb and had 325 cc high profile cohesive silicone gel microtextured implants placed in a dual plane position through an inframammary incision (at the breast fold) combined with a periareolar mastopexy using a round-block Goretex suture.
Discussion: Her breasts are very atrophic (thinned) after her pregnancies and breast feeding. Her nipples prior to surgery are below the breast fold and so a mastopexy (lift) is needed. The distance from the bottom of her areola to the fold is not significantly increased however, it is 9 cm on stretch. So she is a candidate for a Vertical lift ( “lollipop scar”) which was our original plan. At the time of surgery, after placing her implants, I felt that we could accomplish her goals with a peri areolar Mastopexy (“circle lift” ). The peri areolar mastopexy is only possible in very few cases, because it does not give much of a lift and it flattens the breast. But in a case where the breasts are narrow / “pointy” as we have here, it improves the shape of the breast. In a breast that is already wider at the base it would tend to make the breast “boxy”. But in her case it was just right. This is also called a “concentric circle” mastopexy because a larger circle that reaches to the top of where we want the areola to go is drawn around a second circle that defines the new areola. A goretex suture that is permanent is used to prevent the areola from stretching out to the size of the larger circle. It “blocks” the areola from stretching out.
Although we could have placed her implants through the peri areolar incision and avoided the inframammary incision, her tissues are very thin, and I felt that is was safer to keep the space where her implant was placed separated from the incision around her nipple. This decreases the risk of the implant becoming exposed if the incision were to separate after surgery. It also avoids having to split the breast tissue which has breast ducts and bacteria, giving a higher risk of capsular contracture when the implant is placed through the peri areolar incision.
A high profile implant was used. In a tight breast it might appear overly “bulgy” on top, known as “superior pole convexity”. But in a loose breast that is deflated as we have here it is usually good to try and replace some of the lost volume with a higher profile implant. We are trying to “fill” the breast without overly stretching it.
A micro-textured implant was used. Smooth Implants tend to drop and fall off to the side with time, especially in a loose, stretchy breast. Texture may help to prevent this shifting of the implant. Texture can be controversial however because it could increase the risk of BIA-ALCL, which has only been reported in textured implants. It is felt to be an interaction of Biofilm when bacteria gets on the implant, with the texture. The risk of BIA-ALCL is very low however, is very treatable when recognized, and is more common in the aggressively textured implants. It is less common in the micro-textured implants, that have a less aggressive texture. So if we are going to use texture, I feel that the micro-texture is my choice, and of course we use our “14 steps” to avoid bacterial contamination of the implant.
The dimensions of the implant were carefully selected based on her tissue dimensions and confirmed by her in a bra with the Mentor sizing system in the office.
So, a lot of thought and planning to size the implant properly, pick the implant profile and texture and plan the surgical approach. There is no right or wrong way to do this surgery. But these are the tradeoffs that the patient and I together decided were best in her particular case.
This is an early result, and we can expect the breasts to settle and the scars to fade over the following months. But her case illustrates some of the tradeoffs that go into planning a mastopexy augmentation












Cosmetic & Plastic Surgery Specialist
"I treat my patients like I would treat
- Jonathan D. Hall, MD, FACSmembers of my own family."
Schedule Consultation